Laparoscopy
Your frequent questions
What are the advantages over open surgery?
Laparoscopy is also performed under general anaesthetic. Nevertheless, thanks to the mini-invasive surgical approach (incisions of only a few millimeters), recovery is generally rapid and post-operative pain limited. Laparoscopy reduces scarring, lowers the risk of adhesions, promotes faster resumption of daily activities and limits the length of hospital stay.
.
What pathologies can be diagnosed or treated by laparoscopy?
In gynecology, laparoscopy is indicated in the management of endometriosis, for the removal of ovarian cysts or certain uterine fibroids, as well as for the treatment of ectopic pregnancies. It is also used to release pelvic adhesions, infertility workup, as well as for more extensive procedures such as hysterectomy or promontofixation in the context of prolapse.
What is the average length of a laparoscopic operation?
The duration of a laparoscopy varies according to the type of procedure performed. A diagnostic laparoscopy takes an average of 20 to 30 minutes, while an operative procedure (e.g. for an ovarian cyst, endometriosis or hysterectomy) can last between 1 and 3 hours. Operating time depends on the complexity of the pathology and the surgical procedure planned.
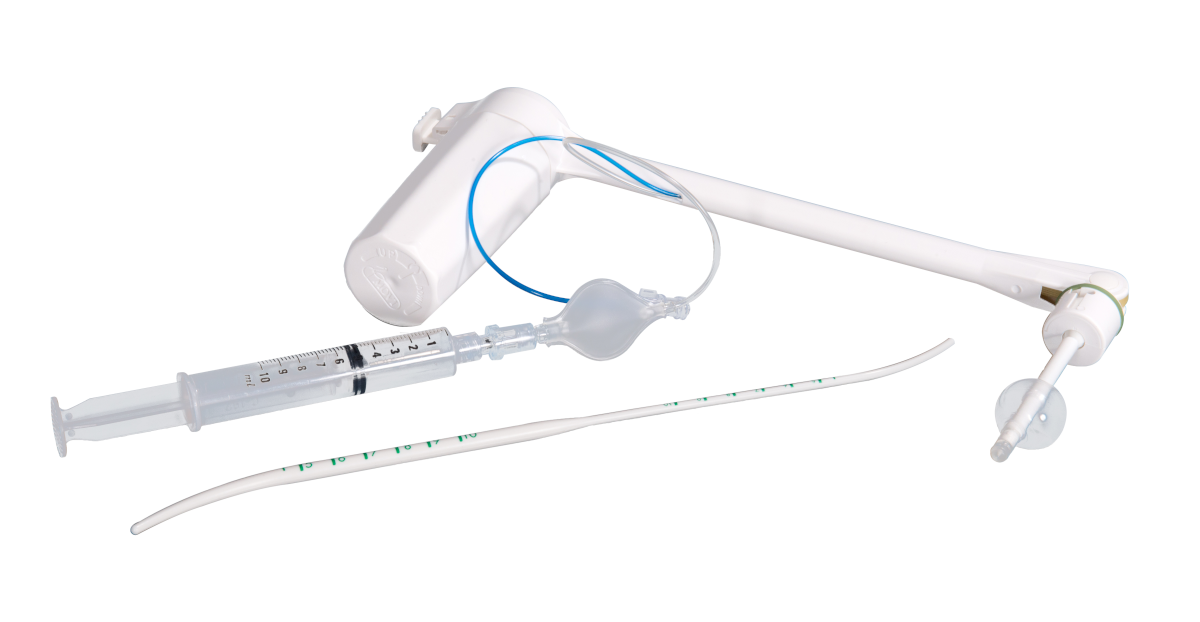
When is the use of a uterine manipulator recommended?
The uterine manipulator is a device used in laparoscopy to mobilize the uterus and offer better visibility of the pelvic organs. Its use is particularly useful when treating deep endometriosis, in uterine fibroid surgery, during hysterectomies or even when exploring infertility. By enabling the uterus to be moved in a controlled manner, it facilitates vision, surgical access and improves the precision of operative gestures.

Laparoscopy, a minimally invasive surgical approach
Laparoscopy, also known as celioscopy, is a minimally invasive surgical technique that allows exploration of the abdominal or pelvic cavity and intervention on various organs: digestive (liver, colon, gallbladder, etc.), reproductive (uterus, ovaries, fallopian tubes), or urinary. It is based on the principle of accessing the organs through small skin incisions, generally 5 to 10 mm, through which a camera and specific instruments are inserted. To create a working space and ensure optimal visibility, the abdominal cavity is distended using a gas, most often CO₂, insufflated at controlled pressure. This process allows the surgeon to visualize the organs without compressing them and to manipulate the instruments safely.

The procedure requires specialized equipment including:
- Trocars serving as access points for inserting instruments,
- A laparoscope connected to a high-definition imaging system providing a magnified and precise image of the abdominal cavity on a screen,
- Surgical instruments adapted to the different surgical procedures,
- An irrigation/suction system to maintain clear visibility by removing blood and debris,
- An insufflator to continuously maintain CO₂ pressure in the abdomen,
A smoke aspirator, necessary when using surgical energies to preserve image quality and the safety of the team,
- And, in some cases, a uterine manipulator to mobilize the uterus to improve exposure of the pelvic organs.
Thanks to this combination of mini-incisions, high-quality imaging, and specialized instruments, laparoscopy offers an alternative to surgery open, allowing to reduce postoperative pain, limit complications and promote a faster recovery.
The essential criteria for a safe laparoscopy
In gynecology, the success and safety of a laparoscopy depend largely on the quality of the instruments used. A reliable and ergonomic uterine manipulator is essential to ensure precise positioning of the uterus and provide the surgeon with optimal exposure of the pelvic organs. The optical quality of the laparoscopes also plays a crucial role, as a high-definition, bright image allows for precise visualization of the tissues and safe guidance of surgical procedures. Thin, durable instruments adapted to specific techniques allow for efficient work while minimizing trauma. Finally, the ergonomics and reliability of the equipment contribute not only to the smoothness of the surgical procedure but also to the overall safety of the intervention.